-
Governance advisory
We guide boards and management teams in frameworks, team processes and leadership dynamics to deliver sustainable value.
-
Financial services advisory
Get market-driven expertise to achieve your goals in banking, insurance, capital markets, and investment management.
-
Business risk services
Our market-driven expertise helps firms keep growing and manage risk in an evolving regulatory landscape.
-
Risk
Meet risks with confidence and transform your business – we support you to manage risk and deliver on your goals.
-
Economic consulting
Bespoke guidance grounded in complex economic theory and practical sector insight to help you make the right decisions.
-
Government and public sector
Experience and expertise in delivering quality public sector advisory and audits.
-
Business consulting
Partnering with you to deliver sustainable business change that helps you realise your ambitions.
-
Transaction advisory services
Whether buying or selling, we help you get the deal done with our comprehensive range of transaction advisory services.
-
Financial accounting advisory services (FAAS)
Our FAAS team can support your finance function with the flexible resource they need to get results.
-
Corporate finance advisory
Building a business is never easy. We help you maximise the value of your business and find the right option.
-
Valuations
Help to understand or support the valuation of a business or asset.
-
Insolvency and global asset recovery
We provide asset tracing and seamless cross-border global recovery for clients.
-
Forensic and investigation services
Market-driven expertise in investigations, dispute resolution and digital forensics.
-
Restructuring
Our restructuring team help lenders, investors and management navigate contingency plans, restructuring and insolvency.
-
Transformation consulting
Is business transformation a priority for your organisation? Our expert insight and guidance can help you achieve it.
-
Pensions assurance
A tailored service that responds to evolving risks and regulations.
-
Accounting services
Optimise your growth with expert accounting services. Contact us today.
-
Royalty and intellectual property (IP) audits
Enhance IP asset protection with our royalty and IP audit services. Expertise in licensing, revenue detection, and compliance improvements.

-
Business consulting
Partnering with you to deliver sustainable business change that helps you realise your ambitions.
-
Corporate Simplification
Release value, reduce compliance complexity, and improve tax efficiency by streamlining your group structure.
-
Economic consulting
Bespoke guidance grounded in complex economic theory and practical sector insight to help you make the right decisions.
-
Financial accounting advisory services (FAAS)
Our FAAS team can support your finance function with the flexible resource they need to get results.
-
Governance advisory
We guide boards and management teams in frameworks, team processes and leadership dynamics to deliver sustainable value.
-
International
Unlock global opportunities with our local expertise and worldwide reach.
-
People advisory
Driving business performance through people strategy and culture.
-
Strategy Group
Successful business strategy is rooted in a clear understanding of the market, customer segmentation and how purchase decisions vary.
-
Respond: Data breach, incident response and computer forensics
Are you prepared for a cyber failure? We can help you avoid data breaches and offer support if the worst happens.
-
Comply: Cyber security regulation and compliance
Cyber security regulation and compliance is constantly evolving. Our team can support you through the digital landscape.
-
Protect: Cyber security strategy, testing and risk assessment
Cyber security threats are constantly evolving. We’ll work with you to develop and test robust people, process and technology defences to protect your data and information assets.

-
Corporate finance advisory
Building a business is never easy. We help you maximise the value of your business and find the right option.
-
Debt advisory
Working with borrowers and private equity financial sponsors on raising and refinancing debt. We can help you find the right lender and type of debt products.
-
Financial accounting advisory services (FAAS)
Our FAAS team can support your finance function with the flexible resource they need to get results.
-
Financial modelling services
Financial modelling that helps you wrestle with your most pressing business decisions.
-
M&A data analytics
We transform and visualise data to present meaningful and clear outputs, enabling you to make better decisions and realise greater value.
-
Operational deal services
Enabling transaction goals through due diligence, integration, separation, and other complex change.
-
Our credentials
Search our transactions to see our experience in your sector and explore the deals advisory services we've delivered.
-
Transaction advisory services
Whether buying or selling, we help you get the deal done with our comprehensive range of transaction advisory services.
-
Valuations
Help to understand or support the valuation of a business or asset.
-
The ESG agenda
Shape your ESG agenda by identifying the right metrics, sustainable development and potential business value impact.
-
ESG driven business transition
Whatever your ESG strategy, we can support your organisation as it evolves while maximising efficiency and profitability.
-
ESG programme and change management
Do you have the right capabilities to drive the delivery of your ESG strategy to realise your targets?
-
ESG risk management
You must protect, comply, understand and influence to successfully manage the risk involved with ESG issues. We can help.
-
ESG strategy, risk and opportunity identification
We can help you clearly define your ESG Strategy, with the risks and opportunities identified and managed.
-
Create value through effective ESG communication
Building trust and engagement with your stakeholders on your ESG strategy.
-
ESG metrics, targets and disclosures
The pressure to report your ESG progress is growing. Do your targets measure up?
-
ESG governance, leadership and culture framework
Make the most of ESG opportunities by effectively embedding your strategy across your organisation.
-
ESG and non-financial assurance
Support your board to be confident in supplying robust information that withstands scrutiny.
-
Transition planning to net zero
Supporting your organisation in the transition to net zero.
-
Actuarial and insurance consulting
We consult extensively to the life insurance, general insurance, health insurance and pensions sectors.
-
Business risk services
Our market-driven expertise helps firms keep growing and manage risk in an evolving regulatory landscape.
-
Financial crime
Helping you fight financial crime in a constantly changing environment
-
Financial services business consulting
Leverage our diverse capabilities to manage challenges and take opportunities: from assurance to transformation
-
Financial services tax
Helping financial services firms navigate the global financial services and funds tax landscape.
-
Regulatory and compliance
Providing an exceptional level of regulatory and compliance to firms across the financial services industry.
-
Corporate intelligence
Corporate intelligence often involves cross-border complexities. Our experienced team can offer support.
-
Litigation support
Industry-wide litigation support and investigation services for lawyers and law firms.
-
Disputes advisory
Advising on quantum, accounting and financial issues in commercial disputes.
-
Forensic investigations and special situations
Do you need clarity in an uncertain situation? If you're accused of wrongdoing we can help you get the facts right.
-
Forensic data analytics
Our forensic data analytics team are helping businesses sift the truth from their data. See how we can help your firm.
-
Monitoring trustee and competition services
Monitoring trustee services to competition, financial and regulatory bodies.
-
Financial crime
Supporting your fight against financial crime in an ever-changing environment
-
Whistleblowing and investigation support
Whistleblowing frameworks provide many benefits – find out how to build trust and manage risks in a confidential, cost-effective, robust way.
-
Public sector advisory
To deliver excellent public services, local and central government need specialist support.
-
Public sector consulting
Helping public sector organisations maintain oversight of services and understand what's happening on the ground.
-
Public sector audit and assurance
As a leading UK auditor, we have unparalleled insights into the risks, challenges and opportunities that you face.
-
Competition damages and class actions
Helping you recover damages owed from anti-competitive practices.
-
Contentious estates and family disputes
We manage complex and sensitive disputes through to resolution.
-
Digital Asset Recovery
Get guidance and technical expertise on digital finance and cryptoasset recovery from our dedicated crypto hub.
-
Grant Thornton Offshore
Grant Thornton Offshore is our one-stop global solution for insolvency, asset recovery, restructuring and forensics services.
-
Insolvency Act Portal
Case information and published reports on insolvency cases handled by Grant Thornton UK LLP.
-
Litigation support
Industry-wide litigation support and investigation services for lawyers and law firms.
-
Personal insolvency
We can support you to maximise personal insolvency recovery and seek appropriate debt relief.
-
South Asia business group
We help Indian companies expand into the UK and invest globally. We also help UK companies invest and operate in India.
-
US business group
Optimise your trans-Atlantic operations with local knowledge and global reach.
-
Japan business group
Bridging the commercial and cultural divide and supporting your ambitions across Japan and the UK.
-
Africa business group
Connecting you to the right local teams in the UK, Africa, and the relevant offshore centres.
-
China-Britain business group
Supporting your operations across the China – UK economic corridor.
-
Asset based lending advisory
Helping lenders, their clients and other stakeholders navigate the complexities of ABL.
-
Contingency planning and administrations
In times of financial difficulty, it is vital that directors explore all the options that are available to them, including having a robust ‘Plan B’.
-
Corporate restructuring
Corporate restructuring can be a difficult time. Let our team make the process simple and as stress-free as possible.
-
Creditor and lender advisory
Whether you're a creditor or lender, complex restructurings depend on pragmatic commercial advice
-
Debt advisory
Our debt advisory team can find the right lender to help you in restructuring. Find out how our experts can support you.
-
Financial services restructuring and insolvency
Financial services restructuring and insolvency is a competitive marketplace. Our team can help you navigate this space.
-
Pensions advisory services
DB pension-schemes need a balanced approach that manages risk for trustees and sponsors in an uncertain economy.
-
Restructuring and insolvency tax
Tax will often be crucial in a plan to restructure a distressed business. Our team can guide you through the process.
-
Restructuring Plans
Market leading experience in advising companies and creditors in Restructuring Plan processes.

-
Artificial intelligence
Our approach to the design, development, and deployment of AI systems can assist with your compliance and regulation.
-
Controls advisory
Build a robust internal control environment in a changing world.
-
Data assurance and analytics
Enhancing your data processes, tools and internal capabilities to help you make decisions on managing risk and controls.
-
Enterprise risk management
Understand and embrace enterprise risk management – we help you develop and connect risk thinking to your objectives.
-
Internal audit services
Internal audit services that deliver the value and impact they should.
-
Managing risk and realising ESG opportunities
Assess and assure risk and opportunities across ESG with an expert, commercial and pragmatic approach.
-
Project, programme, and portfolio assurance
Successfully delivering projects and programmes include preparing for the wider impact on your business.
-
Service organisation controls report
Independent assurance provides confidence to your customers in relation to your services and control environment.
-
Supplier and contract assurance
Clarity around key supplier relationships: focusing on risk, cost, and operational performance.
-
Technology risk services
IT internal audits and technology risk assurance projects that help you manage your technology risks effectively.

-
Capital allowances (tax depreciation)
Advisory and tools to help you realise opportunities in capital allowances.
-
Corporate tax
Helping companies manage corporate tax affairs: delivering actionable guidance to take opportunities and mitigate risk.
-
Employer solutions
We will help you deliver value through your employees, offering pragmatic employer solutions to increasing costs.
-
Financial services tax
Helping financial services firms navigate the global financial services and funds tax landscape.
-
Indirect tax
Businesses face complex ever changing VAT regimes, guidance and legislation. We can help you navigate these challenges.
-
International tax
Real-world international tax advice to help you navigate a changing global tax landscape.
-
Our approach to tax
We advise clients on tax law in the UK and, where relevant, other jurisdictions.
-
Private tax
Tax experts for entrepreneurs, families and private business. For now and the long term.
-
Real estate tax
Stay ahead of real estate tax changes with holistic, tax-efficient solutions.
-
Research and development tax incentives
We can help you prepare optimised and robust research and development tax claims.
-
Tax dispute resolution
We make it simple to stay compliant and avoid HMRC tax disputes
-
Tax risk management
We work with you to develop effective tax risk management strategies.
-
Skills and training
Get the right support to deliver corporate and vocational training that leads the way in an expanding market.
-
Private education
Insight and guidance for all businesses in the private education sector: from early years to higher education and edtech.
-
Facilities management and property services
Get insight and strategic support to take opportunities that protect resilience and drive UK and international growth.
-
Recruitment
Helping recruitment companies take opportunities to achieve their goals in a market where talent and skills are key.
-
Food and beverage (F&B)
We can help you find the right ingredients for growth in your food and beverage business.
-
Travel, tourism and leisure
Tap into our range of support for travel, tourism and leisure businesses in this period of challenge and change.
-
Retail, e-commerce and consumer products
With multiple challenges and opportunities in the fast-evolving retail sector, make sure you are ready for them.
-
Banking
Our expertise and insight can help you respond positively to long term and emerging issues in the banking sector.
-
Capital markets
2020 is a demanding year for capital markets. Working with you, we're architecting the future of the sector.
-
Insurance
Our experienced expert team brings you technical expertise and insight to guide you through insurance sector challenges.
-
Investment management
Embracing innovation and shaping business models for long-term success.
-
Pensions
Pension provision is an essential issue for employers, and the role of the trustee is becoming increasingly challenging.
-
Payments advisory and assurance
Payment service providers need to respond to rapidly evolving technical innovations and increased regulatory scrutiny.

-
Central and devolved government
Helping central and devolved governments deliver change to improve our communities and grow our economies.
-
Infrastructure and transport
Delivering a successful transport or infrastructure project will require you to balance an often complex set of strategic issues.
-
Local government
Helping local government leverage technical and strategic expertise deliver their agendas and improve public services.
-
Regeneration development and housing
We provide commercial and strategic advice to assist your decision making in pursuing your objectives.
-
Health and social care
Sharing insight and knowledge to deliver transformation and improvement to health and social care services.
-
Charities
Supporting you to achieve positive change in the UK charity sector.
-
Education and skills
The education sector has rarely faced more risk or more opportunity to transform. You need to plan for the future.
-
Social housing
We are committed to helping change social housing for the better, and can help you make the most of every opportunity.

-
Technology
We work with dynamic technology companies of all sizes to help them succeed and grow internationally.
-
Telecommunications
Take all opportunities to realise your goals in telecommunications: from business refresh to international expansion.
-
Media
Media companies must stay agile to thrive in today’s highly competitive market – we’re here to support your ambitions.
-
Career development
The support you need will vary throughout your career, here are just some of the ways we'll support you to you excel with us.
-
How we work
Our approach to how we work, ensures that when we are making choices about how, where or when we work, we have the support and tools we need.
-
Reward and benefits
We are committed to building a culture where our people have access to the necessary benefits to help promote a healthy lifestyle and thrive.
-
Inclusion and diversity
Included and valued for your difference is how everyone should feel at work. Not just because it’s right, but because we’re all at our best when we’re able to be ourselves.
-
ESG: environment and community impact
Our ESG framework enables responsible, sustainable, and ethical operations. We prioritise the environment, our broader societal impact, and our firm's governance to protect the planet, foster inclusivity and wellbeing, support our communities, and bolster our firm's resilience.
-
What we do
It’s an exciting time to be joining Grant Thornton, especially as a trainee at the start of your career. Learn about our teams and the work we do.
-
Life as a trainee
Everything you need to know about life as a trainee, from the experiences you'll get to the skills you need.
-
Employability hub
Our employability hub is designed to help you feel prepared for the application process, and guide you through the decisions you will need to make throughout.
-
Our programmes
Whether you are looking to join us straight from school or with a degree, or even looking for some work experience, we have a programme that is right for you.
-
Parents, carers and teachers hub
Access information and support to help inform career discussions with your young people.
-
FAQs
We hope you can find all the information you need on our website, but to help we've collated a few of the questions we hear quite frequently when speaking to candidates.
-
Advisory
Our advisory practice provides organisations with the advice and solutions they need to unlock sustainable growth and navigate complex risks and challenges.
-
Audit
Every day our audit teams help people in businesses and communities to do what is right and achieve their goals.
-
Tax
The tax landscape is evolving, and our clients need us more than ever to navigate the complexities with them.
-
Central Client Service
From finance and information systems, to marketing and people teams we have a diverse range of teams supporting our business.
-
Our recruitment process
We strive to ensure our interview process is barrier free and sets you up for success, as well as being wholly inclusive and robust. Learn about our process here.
-
International hiring
Our international talent is an important part of our firm, joining us you will be joining a growing community of international hires.
-
Armed forces
As an Armed Forces Friendly organisation we are proud to support members of the Armed Forces Community as they develop their career outside of the Armed Forces.
Having emerged from the worst of the COVID-19 pandemic, NHS finances have come under sustained pressure as the service deals with multiple challenges, including rising waiting lists, high inflation, workforce gaps, industrial action, and a creaking infrastructure. Our analysis earlier in the year identified the underlying drivers of financial performance in 2022/23 and these were flagged as clear risks to delivery during the 2023/24 planning process.
Key insights from NHS audits
Our audits of the 2022/23 NHS accounts include judgements on financial sustainability and governance, as part of the responsibility to assess Value for Money (VfM) arrangements outlined by the Audit Code of Practice. We've used information from the Auditor’s Annual Report (AAR) for 58 NHS trusts where Grant Thornton is the external auditor to highlight the principle challenges for NHS finances.
Financial performance of NHS Trusts is significantly deteriorating
Deficits doubled in value when comparing 2022/23 actuals to 2023/24 plans, with financial distress particularly evident across the acute sector. This is on the back of short-term, non-recurrent measures propping up the 2022/23 position of many Trusts.
41% of NHS Trusts have significant weaknesses in financial sustainability and governance
This is a material increase compared with 2021/22 (10%) – auditor assessments were worse at our NHS trust acute audited bodies where 63% had significant weaknesses identified. The main causes of these assessments were the lack of detailed Cost Improvement Plans (CIPs) for 2023/24 and the existence and maturity of medium term financial plans.
The CIP target included in 2023/24 plans was 65% higher than that delivered in 2022/23. Plans showed this increase would be delivered wholly from recurrent savings. The average CIP target was 5% of income, but there was a range from 2.7% to 9.1% across the 58 Trusts.
Many Trusts had under-developed recurrent and medium-to-long term programmes to bridge planning gaps in their finances. Almost half of savings delivered in 2022/23 were non-recurrent, one-off cost reductions, such as centrally held non-recurrent funding, unspent reserves, and balance sheet adjustments. The majority of Trusts we audited had underlying, operational deficits (up to £150 million in our sample) but no agreed plans with system partners for medium term financial sustainability.
Financial performance
The financial performances of Trusts are deteriorating significantly. From the sample of audited bodies analysed, planned deficits (agreed with NHS England) in 2023/24 total £521 million compared to actual reported deficits of £249 million in 2022/23 – a doubling of deficits in one year.
The underlying position is considerably worse. It's widely reported that financial plans in 2023/24 are challenging and that Trusts and auditors have identified significant risks with their delivery. The use of short-term, non-recurrent measures also propped up the 2022/23 position of many Trusts. The most recent financial report from NHS England already identified overspending of £809 million at month four (July) against these plans.
Our analysis shows continuing widespread financial pressure on the NHS acute sector, with community, and mental health Trusts performing better.
NHS Trust surplus/(deficit) 2022/23 actuals – 2023/24 plans

Source: VFM audit findings as reported in the Grant Thornton 2022/23 Annual Audit Report for 58 Trusts, comprising 35 acute, 11 mental health, 6 community, and 6 specialist Trusts.
Financial sustainability
For 2022/23, our auditors have materially increased the number of significant weakness judgements for financial sustainability, compared with 2021/22. 41% of our Trust audited bodies had financial sustainability significant weaknesses reported - a significant increase from the previous year (10%). Approximately 63% of our acute trust audited bodies received significant weakness judgements – reemphasising that this is a key sector of financial distress.
Summary of financial sustainability findings from VfM audits
 Source: VFM audit findings as reported in the Grant Thornton 2022/23 Annual Audit Report for 58 Trusts
Source: VFM audit findings as reported in the Grant Thornton 2022/23 Annual Audit Report for 58 Trusts
In total, auditors made 119 recommendations to improve financial sustainability and financial governance across the 58 NHS trust audited bodies. More than two thirds of Trusts have recommendations relating to 2023/24 Cost Improvement Plans (CIP) and delivery, and the development of longer-term financial plans. Auditors also identified improvements to financial reporting around the quality of reporting of system financial performance to boards, use of costing information, improvements to monthly finance reports, and clarity of reporting of assumptions, risks and scenarios. They also highlighted the use of short-term financial fixes, such as one-off non-recurrent schemes and technical, balance sheet adjustments, and reviews to underpin financial performance.

Source: VFM audit recommendations, both key and improvement, as reported in Grant Thornton 2022/23 Auditor's Annual Reports for 58 Trusts
Cost improvement planning and delivery
Across 58 Trusts, the CIP target included in 2023/24 plans is £607 million higher (65%) at £1.5 billion compared with £932 million delivered in 2022/23. Plans showed this increase would be delivered wholly from recurrent savings. On average, the CIP challenge in 2023/24 equates to 5% of income, with this ranging from 2.7% to 9.1% across the 58 Trusts. This very large increase in CIP in 2023/24 is happening at a time of continuing operational difficulties with urgent and emergency care, as well as cost-of-living and workforce challenges.
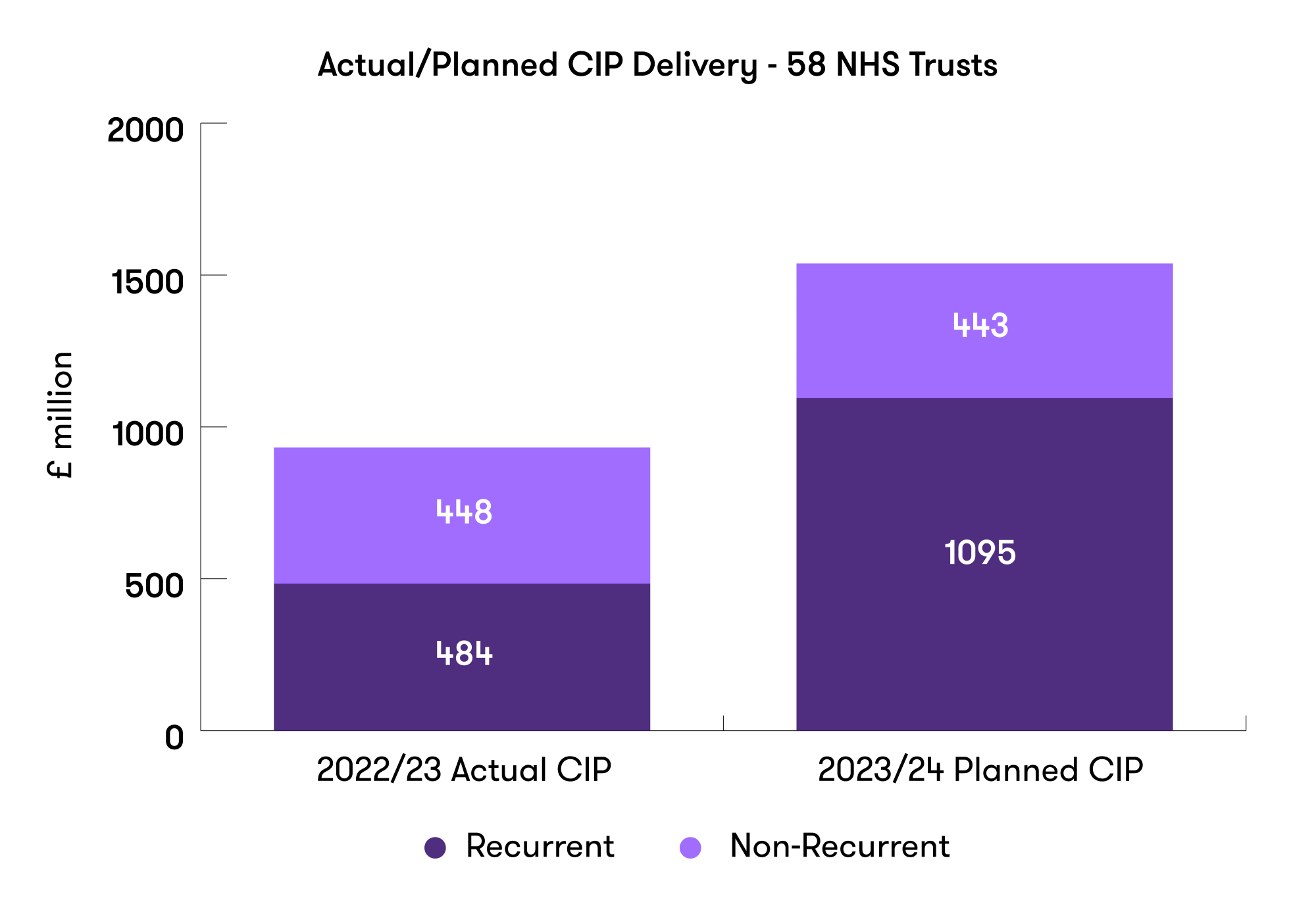
Source: VFM audit findings as reported in the Grant Thornton 2022/23 Auditor's Annual Report for 58 Trusts
During 2022/23 Trusts returned their focus to operational productivity, with workforce growth compared against pre-pandemic levels being a key area of focus.
Many Trusts had under-developed recurrent and medium to long-term programmes to bridge planning gaps in their finances. They also had ineffective monitoring arrangements for tracking the financial impact of operational productivity improvements at a Trust and system level. Trust schemes are still generally aspirational, temporary, and non-recurrent. There's also limited evidence of system-wide productivity measures delivering significant benefits. Much more work still needs to be done to deliver significant cost and waste savings through system collaboration to build financially sustainable plans.
Almost half of savings delivered in 2022/23 were non-recurrent, with examples of one-off cost savings including centrally held non-recurrent funding and unspent reserves - largely as a result of the COVID-19 funding regime: VAT reviews, releasing provisions and other balance sheet adjustments. These short-term, non-recurrent measures were a key area of focus for audit testing and don't contribute to creating longer term financial sustainability.
Medium term-financial planning
The majority of Trusts we audited had underlying, operational deficits (up to £150 million in our sample) and no agreed plans with system partners for medium term financial sustainability. Non-recurrent funding and adjustments continue to obscure the underlying operational financial position of many hospitals. Understanding the true financial baseline and drivers of performance is the starting point for financial sustainability.
Detailed three to five year financial plans can help demonstrate the scale of financial turnaround required and set the stage for clinical, workforce, and operational plans and strategies. This shouldn’t be something that's only produced for regulators – it’s a fundamental component of service management and planning.
Reviewing long term operational and financial plans (including long term CIP programmes) – and regularly updating them needs to become business as usual and not just part of the annual planning process. This will help to broaden the understanding of the risks and challenges with clinical and operational leadership as well as regulators. Financial plans need to be underpinned by models showing the impact of service changes, investments and transformation, and productivity programmes with scenario planning. To be credible it's vital that there's genuine triangulation of operational performance and activity, workforce, quality impact, and finances.
Delivering financial sustainability
Financial plans for 2023/24 included stretching targets and optimistic assumptions, with most Trusts reflecting significant risks to delivery. Already we're starting to see clear warning signs that Trusts and systems are struggling to hit year-to-date targets and the re-emergence and appointment of turnaround directors in systems which are financially challenged. Our analysis does suggest several actions that successful NHS Trusts will take.
Getting back to basics
Ensuring key information and data is updated and accurate so there's a clear understanding to build reliable analysis on, including demand and capacity modelling, costing, service line reporting, data and coding accuracy, and workforce information and analysis.
Understanding the real operational financial position
Stripping out non-recurrent income and costs and ensuring workforce is the right size for agreed activity plans and productivity plans. Evaluating contribution and service level financial performance.
Maintaining and restoring financial control and process
Ensuring the whole organisation manages its overall spending effectively by reinforcing the need for strong financial control.
Investing in developing and delivering multi-year, recurrent cost improvement programmes
Both Trusts and wider systems need to work together to deliver three to five year plans by providing capacity and joining up work to develop long term opportunities to balance the books. Establishing effective management and monitoring arrangements to ensure these are tracked and provide assurance over their delivery.
Effective engagement and ownership with clinical and operational teams
Working with clinical and operational leaders to provide an understanding of the overall financial picture, spending issues and patterns, and supporting the need for efficiency and delivering programmes.
Developing a medium-term financial plan
In our experience few Trusts have a clear and detailed medium term financial plan over the medium/long term. The need to develop this working alongside system partners is a key requirement to build and restore confidence in Trust plans and deliver financial sustainability. A medium/long-term financial model can also be a useful tool to shift focus on to the challenges beyond the current year and can really help Directors of Finance to quickly show the multi-year impact of different assumptions and scenarios.
What can NHS Trusts learn from these findings?
All of these actions have to be balanced against the need to deliver safe patient care, timely access to services, and the sustained day-to-day operational pressures that the NHS faces. It's no wonder NHS leaders are scratching their heads on how this all can be achieved. And as challenging as it is, transparency and understanding of the financial position are critical in interactions with boards, regulators, and auditors.
For more insight and guidance, get in touch with Peter Saunders, Emily Mayne, and
Nick Caley.






